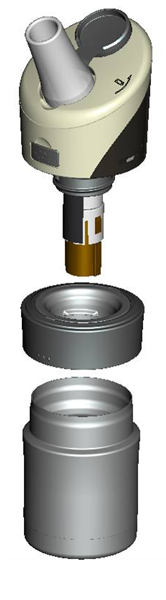
Studies have indicated a correlation between the onset of asthmatic episodes and a rise in exhaled breath temperature. Studies have been initiated to further clarify and quantify this relationship. The device is currently in the published phase of its PCT patent application, with national patents currently being prosecuted in all relevant markets.
During the last decades of the past century the concept of airway inflammation as underlying feature of asthma has became the basis of our understanding and management of this chronic disease. This came as a result of invasive methods of investigation (bronchoscopy with alveolar lavage and biopsy), and was further reinforced by non-invasive methods like sputum analysis, measurement of nitrogen oxide in the exhaled breath, measurement of inflammation mediators in exhaled breath condensates. However, these methods are time consuming, expensive and difficult to standardize.
Inflammation is a universal pathological reaction and is characterized among other things by increased heat production / higher temperature. The question stays whether the inflamed lung airways contribution to the overall exhaled breath temperature can be detected and differentiated by the “white noise” of confounding factors. Paredi et al. (1) and Piacentini et al. (2) have measured the temperature of the exhaled breath of subjects while measuring their level of the exhaled nitric oxide used temperature sensors in front of their mouths. This approach to measure exhaled breath temperature is rather sophisticated and difficult to standardize, but still the authors have found an association between the amount of the exhaled nitrogen oxide and the features of the temperature of the exhaled air.
We have managed to gather data on the exhaled breath temperature of healthy volunteers and asthmatics.
1. We measured the repeatability of exhaled breath measurements of in 11 healthy volunteers at the same time on consecutive days using repeated measures analysis. The intra item correlation turned out to be excellent (≈0.99). Its correlation with atrial (ear) and axillar temperature was low, suggesting that it is measuring a different and more consistent physiological variable (Table 1).
Table 1: Reliability Statistics
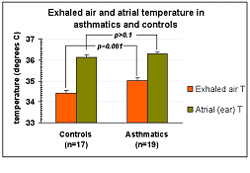
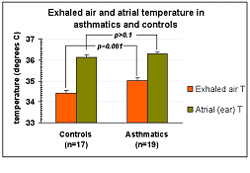
2. We also compared the morning exhaled breath temperature of 19 asthmatics and 17 non-asthmatics by independent samples t-test (Figure 1). There was a difference between the exhaled air temperature of asthmatics (mean 34.41 ± s.e.m. 0.27°C) and controls (35.02 ± 0.21°C), but there was considerable overlap (p=0.081). It should be stated that most of the asthmatics studied were relatively well controlled on inhaled corticosteroids.
Figure 1
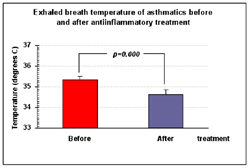
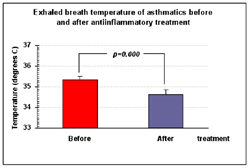
There was a significant difference between the exhaled air temperature of asthmatics before (mean 35,33 ± s.e.m. 0.17°C) and after improvement under anti-inflammatory treatment (34,64 ± 0.21°C), (p=0.000). (Figure 2).
Figure 2
Conclusions
The device we constructed can measure the temperature of exhaled air in human subjects in a simple and acceptable non-invasive and user-friendly way. Further experiments are warranted to find out if it can be applied as individual device for asthmatics to assess the degree of control of their airway inflammation. Studies in other lung diseases may provide support about the validity and usefulness of the method in chronic and infectious pulmonary diseases.
References
Paredi P, Kharitonov SA, Barnes PJ. Faster rise of exhaled breath temperature in asthma: a novel marker of airway inflammation? Am J Respir Crit Care Med 2001; 165: 181–184.
Piacentini GL, Bodini A, Zerman L, et al. Relationship between exhaled air temperature and exhaled nitric oxide in childhood asthma. Eur Respir J 2002; 20: 108–111.
During the last decades of the past century the concept of airway inflammation as underlying feature of asthma has became the basis of our understanding and management of this chronic disease. This came as a result of invasive methods of investigation (bronchoscopy with alveolar lavage and biopsy), and was further reinforced by non-invasive methods like sputum analysis, measurement of nitrogen oxide in the exhaled breath, measurement of inflammation mediators in exhaled breath condensates. However, these methods are time consuming, expensive and difficult to standardize.
Inflammation is a universal pathological reaction and is characterized among other things by increased heat production / higher temperature. The question stays whether the inflamed lung airways contribution to the overall exhaled breath temperature can be detected and differentiated by the “white noise” of confounding factors. Paredi et al. (1) and Piacentini et al. (2) have measured the temperature of the exhaled breath of subjects while measuring their level of the exhaled nitric oxide used temperature sensors in front of their mouths. This approach to measure exhaled breath temperature is rather sophisticated and difficult to standardize, but still the authors have found an association between the amount of the exhaled nitrogen oxide and the features of the temperature of the exhaled air.
We have managed to gather data on the exhaled breath temperature of healthy volunteers and asthmatics.
1. We measured the repeatability of exhaled breath measurements of in 11 healthy volunteers at the same time on consecutive days using repeated measures analysis. The intra item correlation turned out to be excellent (≈0.99). Its correlation with atrial (ear) and axillar temperature was low, suggesting that it is measuring a different and more consistent physiological variable (Table 1).
Table 1: Reliability Statistics
| Common Mean | 34,104 |
| Common Variance | 1,418 |
| True Variance | 1,407 |
| Error Variance | ,011 |
| Common Inter-Item Correlation | ,991 |
| Reliability of Scale | ,996 |
| Reliability of Scale (Unbiased) | ,997 |
2. We also compared the morning exhaled breath temperature of 19 asthmatics and 17 non-asthmatics by independent samples t-test (Figure 1). There was a difference between the exhaled air temperature of asthmatics (mean 34.41 ± s.e.m. 0.27°C) and controls (35.02 ± 0.21°C), but there was considerable overlap (p=0.081). It should be stated that most of the asthmatics studied were relatively well controlled on inhaled corticosteroids.
Figure 1
There was a significant difference between the exhaled air temperature of asthmatics before (mean 35,33 ± s.e.m. 0.17°C) and after improvement under anti-inflammatory treatment (34,64 ± 0.21°C), (p=0.000). (Figure 2).
Figure 2
Conclusions
The device we constructed can measure the temperature of exhaled air in human subjects in a simple and acceptable non-invasive and user-friendly way. Further experiments are warranted to find out if it can be applied as individual device for asthmatics to assess the degree of control of their airway inflammation. Studies in other lung diseases may provide support about the validity and usefulness of the method in chronic and infectious pulmonary diseases.
References
Paredi P, Kharitonov SA, Barnes PJ. Faster rise of exhaled breath temperature in asthma: a novel marker of airway inflammation? Am J Respir Crit Care Med 2001; 165: 181–184.
Piacentini GL, Bodini A, Zerman L, et al. Relationship between exhaled air temperature and exhaled nitric oxide in childhood asthma. Eur Respir J 2002; 20: 108–111.